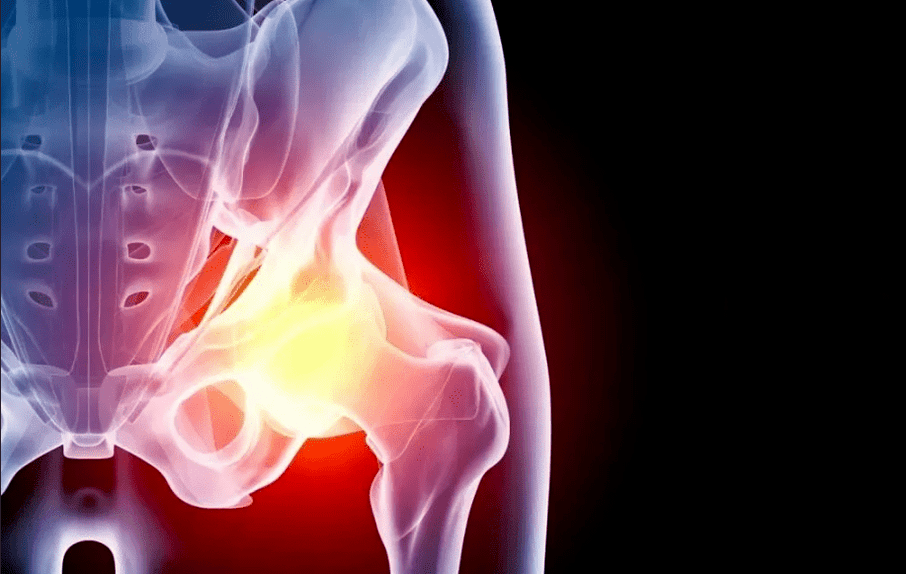
Arthrosis of the hip joint (coxarthrosis) is a chronic pathology, accompanied by the gradual destruction of the cartilage tissue of the affected area, followed by the involvement of adjacent structures in the process. The disease requires long-term treatment and, in severe cases, the only way to regain mobility is to replace the joint.
General Information
Coxarthrosis belongs to the group of degenerative diseases. It begins gradually with microscopic changes in the structure of the cartilage. Increased stress, inflammatory diseases, blood supply disorders lead to structural transformations and thinning of the cartilage tissue and, in turn, deform the contours of the joint area. As a result, the load distribution on the contact surfaces of the bones changes, and the zones with the greatest pressure begin to wear out faster. This triggers a whole cascade of pathological reactions:
- the appearance of microfractures and compaction zones in the cartilage tissue;
- decrease in the smoothness of the articular surfaces;
- excessive growth of cartilage at the site of thinning and replacement with bone tissue;
- the appearance of osteophytes (bone growths) along the edges of the joint site;
- thickening and decreased elasticity of the joint capsule;
- hardening and reduced strength of the ligaments;
- changes in the composition of the synovial fluid (natural lubrication within the joint);
- narrowing of the joint space;
- fusion of all elements of the joint (ankylosis).
Without treatment, coxarthrosis inevitably becomes the cause of immobility and disability.
causes
Depending on the causes of the development of the disease, primary and secondary coxarthrosis is distinguished. In the first case, it occurs on its own, for example, against the background of a hereditary predisposition, in the second, it is provoked by other diseases or injuries. In most cases, the cartilage tissue degeneration process occurs due to a combination of several factors. The reason could be:
- congenital dislocation of the hip;
- flat feet, scoliosis and other orthopedic problems;
- Legg-Calve-Perthes disease;
- joint inflammation (arthritis), regardless of its origin;
- injuries and microtraumas of the hip joint against the background of overweight, professional sports, etc. ;
- hip joint dysplasia;
- metabolic disorders;
- endocrine diseases (especially diabetes mellitus);
- violations of the blood supply to the lower extremities;
- frequent stress;
- heredity (coxarthrosis in parents or other close relatives significantly increases the risks of developing it in a child);
- congenital pathologies and autoimmune diseases of the connective tissue (joint hypermobility, rheumatoid arthritis, systemic lupus erythematosus, etc. );
- joint operations immediately.
Age is an important predisposing factor. According to statistics, after 45 years, the likelihood of developing coxarthrosis increases significantly.
Symptoms
The main symptoms of coxarthrosis of the hip joint do not depend on the cause of the development. Most patients notice:
- movement restriction - one of the first symptoms due to thinning of the cartilage layer and increased friction of the articular surfaces of the bones; in the future, the appearance of cartilage growths further exacerbates the problem;
- pain: the friction of the bones deprived of a cartilage layer against each other, the gradual involvement of all elements of the joint in the degenerative process, a decrease in the blood supply to the tissues causes pain sensations that increase with the progression of the disease; the pain is excruciating in nature and often worsens towards the end of the day;
- muscle spasm, leading to increased pain symptoms and limited range of motion in the joint;
- decrease in the length of the legs - this symptom appears in the later stages of the disease due to the narrowing of the joint space and the gradual grinding of the heads of the bones due to constant friction; the difference between the legs can be up to 2 cm;
- lameness - associated with severe pain and limitation of movement, as well as shortening of the leg; it is an unfavorable sign that indicates serious damage to the joint system.
Phases
In the process of development, coxarthrosis goes through several stages, which depend on the degree of tissue damage.
- 1 degree. At this time, the patient notes mild aching pains in the joint that appear after intense or prolonged physical activity and quickly pass after rest. As a rule, discomfort occurs precisely in the area of the hip joint, but in some cases it extends to the hip or knee. The gait does not change, the movements of the legs are preserved in full. On the roentgenogram, specific changes are noted: subchondral sclerosis.
- 2nd degree. The pain becomes more severe, arises after exertion, spreads to the entire thigh and groin. After exertion, a slight lameness may appear. Difficulty is found in abducting the leg. X-ray shows a significant decrease in the distance between the bones (by 50% or more), deformation of the femoral head and pronounced bone growths.
- 3 degrees. The pains become permanent, walking without a cane becomes impossible. When moving, the patient tilts significantly to the painful side, which further increases the load on the joint. The range of motion is reduced, the muscles in the leg and buttocks atrophy. There is a shortening of the affected limb. X-ray reveals significant deformity of the joint, a change in the contour of the femoral head, and a large number of osteophytes.
- 4 degrees. The pain becomes stronger and does not stop for a minute, the patient loses the ability to move independently. The x-ray shows the complete destruction of the articular cartilage, as well as signs of bone fusion with each other (ankylosis). Coping with the disease at this stage is possible only surgically.
Diagnostics
An orthopedic traumatologist is responsible for identifying symptoms and selecting treatment. To diagnose and determine the extent of the disease, you use:
- survey: listening to patient complaints, identifying risk factors (trauma, disease, heredity, etc. );
- examination: assessment of the mobility of the limbs, determination of the areas of greatest pain;
- Radiography - an X-ray image allows you to assess the condition of the bones and cartilage, the size of the joint space, the presence and location of bone growths; to see more deeply the necessary details, the study is complemented by CT (computed tomography);
- laboratory diagnostics: a general blood test allows you to identify signs of an inflammatory process, biochemical - to note some risk factors, for example, the level of uric acid;
- MRI (magnetic resonance imaging) - allows you to assess the condition not only of bones and cartilage, but also of soft tissues: bones, ligaments, muscles, joint capsule, etc. ;
- puncture of the joint.
If it is necessary to carry out differential diagnostics with other diseases, as well as evaluate concomitant pathologies, then additional tests, instrumental examinations and consultations of narrow specialists are prescribed.
Treatment of coxarthrosis
Treatment of hip joint coxarthrosis depends on its stage and the severity of symptoms. Pathology requires an integrated approach that uses various methods:
- Pharmacological treatment;
- non-drug treatment (physiotherapy, physical therapy);
- surgery;
- lifestyle correction and diet.
Pharmacological treatment
Medicines prescribed for osteoarthritis of the hip joint are aimed at:
- removal of pain syndrome;
- restoration or at least slowing of the destruction of cartilage tissue;
- improve blood supply and nutrition to the affected area;
- treatment of concomitant pathologies.
Painkillers are used in the form of tablets, intramuscular and intraarticular injections, and topical agents: creams, ointments, patches. In the early stages of the development of the disease, non-steroidal anti-inflammatory drugs are sufficient for most patients. With severe pain syndrome, hormonal agents are used. The introduction of analgesics directly into the joint capsule has a good effect.
If the course of the disease is accompanied by muscle spasm, muscle relaxants are used. They are used in combination with other analgesics.
The intake of painkillers should be limited in time and dose, so as not to cause further damage to the cartilage tissue and other side effects (in particular, the development of gastritis and gastric ulcers).
Chondroprotectors are drugs that help restore cartilage tissue. They are effective only with long-term regular use, which is combined with other methods of treatment, lifestyle and dietary adjustments. Drugs to improve blood microcirculation help improve their effect. For a similar purpose, warming ointments are prescribed. Only a doctor is involved in the selection of the dosage and regimen.
Drug-free treatment
This category includes various physiotherapy and manual techniques, as well as physiotherapy exercises. They help improve microcirculation and restore movement in the damaged joint. Depending on the situation, the doctor prescribes:
- shock wave therapy;
- magnetotherapy;
- electromyostimulation;
- various types of electrophoresis and phonophoresis (accompanied by the administration of anesthetic drugs);
- mechanotherapy;
- massage and physical therapy.
Surgery
If the disease has reached the stage of development 3-4, then drugs and physiotherapy will only relieve the patient's condition, but will not restore the ability to move completely. In this case, arthroplasty is indicated, eg. complete or partial replacement of the damaged joint with a titanium prosthesis.
If there are indications, a lighter version of the intervention is performed: grinding of the contact areas of the bones and covering with special smooth implants that facilitate sliding.
Prevention
Lifestyle can significantly reduce the risk of developing coxarthrosis, as well as the speed of its progression. It is important to strictly adhere to the rules:
- lead an active lifestyle: swimming in the pool, walking, cycling - physical activity at an amateur level without running for records helps improve blood supply and inhibits the processes of joint degeneration;
- normalize body weight to reduce the load on the legs;
- eliminate injuries, hypothermia and occupational risk factors (vibrations, weight lifting, standing work);
- promptly treat all diseases, including those not directly related to the musculoskeletal system;
- correct posture disorders over time, wear comfortable shoes.
Diet
With the help of nutritional correction, the patient can not only reduce body weight, but also reduce inflammatory reactions, salt deposits in the tissues and metabolic disorders. It is recommended that you stick to a balanced menu with sufficient, but not excessive, amounts of carbohydrates, proteins and fats, as well as vitamins and minerals. Particular attention should be paid to unsaturated fats (olive and linseed oil), omega-3 acids (found in excess in fish), collagen (meat in jelly, jelly). It is recommended to minimize fast carbohydrates, alcohol, strong coffee, products with artificial flavors, preservatives and flavor enhancers.
Consequences and complications
Coxarthrosis is one of the most common causes of disability in older people. Without proper treatment, the pathology inevitably leads to complete disability, especially in bilateral injuries. Pain and limited mobility do not allow you to work and take care of yourself, which is why it is important to receive care on time.














































